Related Resources
For Understanding Trauma
Understanding Trauma (YouTube Playlist)
Dr. Kate Truitt begins by introducing this 37-episode series, where she covers the intricacies of trauma, such as post-traumatic stress injury and complex trauma. This includes addressing questions such as why do some people have PTSD and others don’t, how many adverse childhood experiences do we have and what trauma does to the brain and body.
In this series, we dig deep into how to go from being survivors to becoming thrivers, or learning how to “Phoenix up.” This means taking the experiences of our past and turning them into personal empowerment. The story of the phoenix illustrates a fire bird that flies into flames to burn up. It consistently rises stronger and wiser than ever before. The bird chooses to burn up, so that it can rise, and Dr. Kate explains that this is the opportunity with trauma.
How Traumatic Stress Impacts the Brain
Did you know that your brain is designed to find the difficult moments in every day? Our little friend “Amy” the amygdala loves to search out those hard moments—those difficult experiences that lead to feelings of anxiety, frustration, and sadness.
Counterintuitively, the reason for this is she’s always trying to keep us safe. The unfortunate side effect is that when we have a difficult moment Amy will start spinning worst case scenario stories about these experiences. I like to think of it as a choose your own adventure of doom that our brain will take us on in order to keep us prepared for every eventuality. For anyone who’s ever experienced ruminating thoughts then you know how painful this can be.
Luckily there are easy steps we can take to stop ruminating in its tracks and instead let our amygdala know that we are safe and sound.
Understanding the Impact of Stress & Trauma: The Window of Tolerance
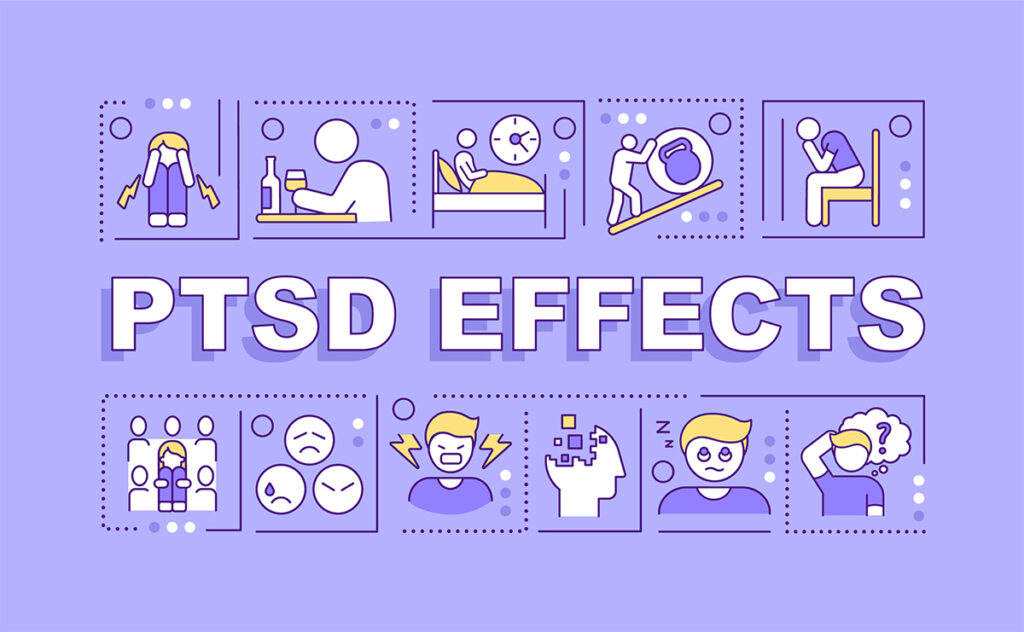
In this psychoeducation video, Dr. Kate Truitt walks us through the window of tolerance and the impact of long-term stress and trauma on the mind and body. She begins by explaining that experiencing a traumatic event can change the way our mind and our body show up in our day to day lives, and it can be for a short time after the trauma or can create long-term change. Our mind and body are a closed loop system, what impacts one impacts the other.
Dr. Kate then explains that the window of tolerance is the body in its optimal state, where it can access both reason and emotion. Outside of the window of tolerance is hyperarousal (over-reactivity, unclear thoughts, emotional distress, anxiety) and hypoarousal (depression, unmotivated, numbness, fogginess, fatigue). When we experience a traumatic event, it can push us out of the window of tolerance to hyperarousal or hypoarousal.
In a healthy mind body system, our system will rebalance. But if we experience a big enough stressor or prolonged stressors, we will start cycling between the red and the grey zone state. This can often look like a cycle between anxiety and depression. If we stay in this cycle, our window of tolerance shrinks.
Dr. Kate reminds us that we have the power of neuroplasticity in our hands!
Taming the Trauma Survival Responses of Fight, Flight, and Freeze
By Dr. Kate Truitt
This is the second in a series of four blog articles about understanding and healing trauma.
Our brain comes equipped with some very powerful coping skills. They come to the fore when we face a threat that seems big or scary enough to endanger our life. And if we’ve encoded a traumatic experience in the past, these coping skills might become a regular part of our day-to-day experience, for better or for worse. The coping skills I’m referring to are the four F’s—fight, flight, freeze and fawn—along with the two D’s—dissociation and defensive rage.
Fight, Flight and Freeze: Powerful Coping skills
In the remaining three articles in this series I will unpack all of these coping skills, how they come to be, what their jobs are, and what they look like in our day-to-day lives. Specifically, in this second article I will focus on the first three of those four F’s: fight, flight and freeze. Let’s start with fight and flight, because these two coping skills have some commonalities in terms of how our body is responding in a moment—they’re both bringing our brain and body online into an activated state to move into action, and to do something different immediately.
Because of those experiences in fight or flight states, our muscles tense and our heartbeat quickens. We begin taking in more air, and other primary organ systems will shut down. We may no longer feel hungry or even feel like we have to use the restroom if those were concerns prior to experiencing the threat. Despite some physiological similarities, these two experiences are experienced very differently. You might imagine that the words fight and flight have some distinct connotations.
Fight: Putting Up Your Dukes and More

When we experience a fight response, we’re putting our dukes up. We’re going to engage whatever the threat is, and try to change the threat in some way, shape or form. Fight often comes up when there is no opportunity to flee, which is that flight coping skill, and when our system knows that freeze is not a viable option.
In extreme cases, fight can take us into that defensive rage that I mentioned earlier. And in fact, our little friend Amy the amygdala has a specific nucleus that gets pinged in fight as well as the defensive rage experiences. And if that little nucleus comes on board in a big way, then we find ourselves in a zoned-out state of rage fighting for our lives.
In our day-to-day existence, on the other hand, fight can manifest itself as irritability, aggression, or stepping over or even crashing through other people’s boundaries. This all comes from a state of feeling threatened down to our very being. It is as though we feel the need to force ourselves on the world around us in order to stay safe. We try to take control, manage, and create what needs to happen, and lash out at anything that might get in our way.
In a moment of threat, fight can be a highly successful coping strategy. Perpetrators may cower, or even go away faced with the power of it. If a dog is chasing us we might turn and stand our ground—waving our arms and making ourselves look bigger and scarier—causing the dog to turn and slink off. This is an example of where it becomes clear to Amy that flight is no longer the best option for keeping us safe and freeze probably will not be an ideal one either, so she changes the coping behavior on the fly, so to speak.
This might be an effective coping strategy in the case of the dog, but living constantly in our daily lives in fight mode is highly taxing on our nervous system and our relationships. So let’s go back to where we were at the beginning with the dog—in flight.
Flight—There’s More to it Than Meets the Eye
Flight is just what it sounds like: we’re running away to get out of a situation. But flight goes far behind the physical manifestations you might imagine. In fact, the day-to-day symptom presentations of flight might surprise you.
Flight can show up much like avoidance—hiding, disconnecting from the world, shutting ourselves down, or numbing out with substances, food, or watching TV. Flight is a way to stay clear of the things that scare us. This can be anything, not just a scary person. If we’ve been in a car accident, cars might put us into flight mode so bad that we avoid interacting with cars at all. (That can seriously inhibit your ability to get around in the world.)
If they’re occurring after a traumatic experience, these are all symptoms that stem from an initial encoding experience in which our brain was trying to keep us safe. In a traumatic experience itself, these behavioral manifestations make sense: Our brains are saying, “This is how I stay alive.”
But there is a point at which this can get messy.
If we’ve successfully avoided a threat enough times through one of these mechanisms in the past, the one that we used can become our go-to, making us default to flight for everything, regardless of the intensity of the threat. And we might default to flight for everything. Remember, our little friend Amy generalizes her data, and her coping skills work the same way.
Freeze! A Common Orienting Response Takes on More Meaning in Trauma

Now let’s dive into that unique phenomenon called freeze, that third “F” you hear about. Frequently, the three are all tied together as fight, flight, and freeze into one construct, but they are actually very different systems interacting within us to create safety in the world.
We all experience freeze on a fairly regular basis. If you’ve ever heard a loud sound, or saw something unexpected and turned quickly to catch it with your eye, pausing to make sense of what it is, that’s a freeze response. It is also known as an orienting response. It’s a method our brain and our body use to create space to make sense of novel stimuli in the environment.
In the context of a traumatic response, though, it turns into something larger. And that same microsecond freeze response takes over our entire system, slowing down our heart rate and our breath, turning our system into a state of calm and quiet while our vision and full awareness focus in on the perceived threat, whatever that might be. The idea is for us to be as quiet, small, and silent as possible, almost as though we’re trying to become invisible.
That makes sense in the face of a perpetrator when we know that fighting isn’t an option and if we run they’ll come after us. The freeze response can become a viable option for children when they living in a chaotic or dangerous environment—when they know that no matter what they do, that perpetrator is going to grab them, because as children, they are vulnerable.
When our system has learned or experienced a mechanism of survival enough times, the fact that we’re re-experiencing that survival mechanism means it keeps working. Because we keep surviving, that can become a go-to mechanism. Over the course of time, we are building in a natural freeze response in the face of any perceived threat. It doesn’t have to be real, just something that is causing our brain to say, “Hey, that reminds me of something that was scary, or could be scary.” Whether that’s something was scary now or 25 years ago, that response becomes ingrained, and we shut down, disconnect, and go into a freeze state.
In polyvagal theory, we talk about the dorsal vagal response (Porges, 2009). And that’s what this is, the entire system shutting down. It can take quite some time to mobilize back into movement, and it can be very scary to be in this space. We are simply moving out of the reality that we’re in and we’re unable to create change or make movement. A lot of my patients who have the freeze response have also developed depression, lethargy, fatigue—a slow-moving space in the world around them that rides shotgun with feelings of helplessness and shame.
Being in a freeze response is very complicated and painful. It can feel like we can’t make a change in the world around us and we’re at the mercy of whatever is going to happen. An important part of recovering from living or in or repeatedly experiencing the freeze response is finding agency meaning and purpose. And agency can be something so small as putting on running shoes in the morning with the possibility of maybe, possibly taking a walk. Those little micro movements of change let our system know that we can move forward and do something different.
In extreme forms, freeze can become dissociation and I’ll present more about that in the fourth and final article in this series. If you’re experiencing fight, flight or freeze, remember to lean in with self-compassion. Shame ups the ante on those responses. And when we recognize, “Hey, mind, body, you’re just keeping me alive.” That in and of itself lessens the shame and enhances self-compassion, which then starts to encourage movement, agency and motivation. That’s moving the healing journey forward.
So, here is how you’ll know if you are caught in fight, flight or freeze behavioral patterns: Just go back and review the symptoms and behavioral responses above. Those are your signs. Then notice: Are you engaging in any of those behaviors or any like behaviors?
The good news in this is your brain keeping you safe, which means we have the tools to help Amy feel better: applying that Havening touch and doing the CPR for the Amygdala® when you notice that behavior showing up. These responses always have some sort of energetic presence in our body. Get to know what that feels like and then lean in with self-love. Give your brain a high-five: “Thank you for keeping me safe.” And then choose to do something different in that moment, creating your own exposure paradigms to create functional change in your life.
We have the power of self-healing in our hands with the mindful touch of The Havening Techniques. If you want to read more about this healing opportunity, continue from the September blog article above into our October 2022 blog article titled, The Havening Techniques: New Neuroscientific Insights Shine Light on Ancient Healing Practices.
If you are interested in building your own personalized self-healing journey, check out my book titled, “Healing in Your Hands: Self-Havening Practices to Harness Neuroplasticity, Heal Traumatic Stress, and Build Resilience,” released in December and available on Amazon.